 Someone recently landed on my blog using the search term “how to get a Dexcom approved by Medicare.” If you want to believe the standard line that Medicare doesn’t cover a CGMS, then I suggest you not waste your time reading this article. If you aren’t willing to accept the standard answer, then keep reading. I am on Medicare and have a Medicare Advantage Plan. Guess what, they paid for both a Freestyle Navigator and a Dexcom.
Someone recently landed on my blog using the search term “how to get a Dexcom approved by Medicare.” If you want to believe the standard line that Medicare doesn’t cover a CGMS, then I suggest you not waste your time reading this article. If you aren’t willing to accept the standard answer, then keep reading. I am on Medicare and have a Medicare Advantage Plan. Guess what, they paid for both a Freestyle Navigator and a Dexcom.
If you try to get a CGMS with Medicare, you are going to be told that it isn’t covered. And yes, I heard the “your insurance doesn’t cover that” plenty of times. Abbott told me that when I tried to get the Navigator and Dexcom told me that when I tried to get the Dexcom. Dexcom also told me that even after I had been using the Dexcom for a year and my insurance had been paying for it. I also heard it from supply companies. I have seen that statement made repeatedly on diabetes message boards but if I ask if they tried to file an appeal with their insurance company, they just repeat again that it isn’t covered. Sometimes even with traditional insurance, you have to fight for what you need. Medicare is no different.
When I first tried to get the Navigator, I was told that it wasn’t covered. I knew that before you can file an appeal with your insurance company, something has to be rejected before you can appeal it. The supply company refused to even try to get an authorization from my insurance. Needless to say, I will never use that supply company! I was expecting to have to fight with my insurance company. I was not expecting to get stopped out of the gate by Abbott and the supply company.
I called my insurance company and explained the situation to a customer service rep. I told her that I realized it was not a covered item but they obviously had to reject it before I could file for an appeal. The customer service person at my insurance company told me to have my doctor’s office do the authorization. It would get rejected and I would get my appeal.
 The next problem I wasn’t expecting either. I had talked to my doctor about getting the Navigator. She agreed it was something I should have because I was passing out from low blood sugar. I gave her the paperwork and she signed it and her office faxed it to Abbott. My doctor’s office shouldn’t have been a problem, but I wasn’t expecting to have to deal with the evil Nurse Ratchet there.
The next problem I wasn’t expecting either. I had talked to my doctor about getting the Navigator. She agreed it was something I should have because I was passing out from low blood sugar. I gave her the paperwork and she signed it and her office faxed it to Abbott. My doctor’s office shouldn’t have been a problem, but I wasn’t expecting to have to deal with the evil Nurse Ratchet there.
The doctor’s office was supposed to put the authorization thru and Nurse Ratchet lied and told me it was rejected. I guess she didn’t think that I would call my insurance company to find out what was going on, especially when no one got a letter saying it was rejected. Even then, she continued to sit on her lazy butt and ignored my weekly phone calls to both my insurance and the doctor’s office. Unfortunately in my case, it took getting a black eye after I passed out one day to get Nurse Ratchet to finally do her job. I guess she finally realized she needed to do something when I called to make an appointment for the doctor to look at my black eye and welt on my head.
The doctor’s office finally submitted the authorization for the CGMS. And yes, I did change doctors as soon as I got my CGMS! I hate being lied to. Of course, the CGMS was denied by the insurance, which is what I expected to happen. Once I had the denial, I filed the appeal letter myself. I had everything ready to go other than the blood sugar logs and reference to average blood sugar and standard deviation in my letter. I knew that I could do a better job because I was the one that needed it.
You need to do some leg work yourself. The first thing you need to do is find out what supply company that accepts your insurance also carries the CGMS that you want. When your doctor’s office tries to get the authorization, they usually have to say which supplier you will use. I would first call the companies that you use to get test strips or pump supplies. Once you find a supplier that you can use, then have your doctor’s office put the authorization thru. Once your insurance rejects it, then you can file an appeal. Don’t count on your doctor to do that for you. You are the one that needs it so you can do a better job.
Because a CGMS is not typically covered by Medicare, you need to show why you need it – I say typically because it is not on their list of covered items, but I am not the only person that has gotten one thru Medicare. Look at the forms on the CGMS websites and see what things they have listed as qualifiers for a CGMS and pick the ones that apply to you.
If you have gastroparesis, get a copy of the test results that show you actually have gastroparesis. Gastroparesis can make it fun to control blood sugar, so if you have gastroparesis, that would help qualify you. Having your doctor say you have it without having the testing done will not help you. Studies now say that people who they thought had gastroparesis probably don’t have it. You can read the article that I wrote about that here. Insurance companies read the same studies that we do. The best proof to show that you actually have gastroparesis is providing test results that confirm you have it.
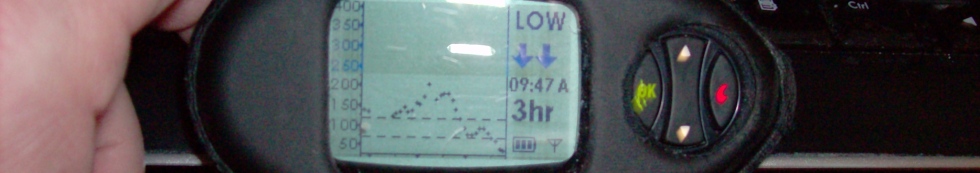
If you have a history of passing out because you are hypo-unaware and don’t feel your lows, get ER records and EMT records to show the trips you have made to the ER because of passing out.
Gastroparesis and passing out because of lows were the two qualifiers for me. Your situation is different than mine. Get medical records to submit to your insurance as proof of your reasons. Provide copies of your blood sugar logs. I have heard some people say to keep the appeal short. I don’t believe that. I believe the more proof you can provide, the better the chance that you will win the appeal. I wrote a very long appeal letter to my insurance company stating all the facts of why I needed a CGMS. In addition to that long letter, I also provided copies of medical records as proof. Someone from my insurance called me when they decided to approve it. They also sent me a letter stating that. During our conversation, she told me that I had a lot of useful information in my letter. Those details do make a big difference.
You don’t have to take no for an answer. Yes you can get a CGMS thru Medicare.
My pump, cgm, and supplies for both are currently covered by the insurance policy I am covered under by my employer. But I am planning on retiring in a few month and will be under COBRA for the next 14 month. So far so good, I will still have all my diabetic supplies covered. However when I turn 65 (July 2013) and go under Medicare it seems I will no longer be covered. Based on your post it seems an appeal letter would be my next step. The problem I have is that I have been fanatical about controlling my blood glucose for twenty plus years and have never had an A1C over 6.2.
I exercise several hours every day (100 plus miles a week on my bike, tennis five days a week, one hour plus walking my dogs every day). I have always tested my BG ten times a day and now with pump and cgm I am down to about seven samples a day. Blood work, eye exams, physicals will all show I am basically not diabetic. But because of this effort to maintain such tight control of my BG I am now asymptomatic for hypoglycemia.
My endocrinologist is very cooperative but I do not see how I could make a case of medical necessity, even though it is because of all the technology that I am able to maintain my BG control.
Any ideas?
Thanks Jerry
Jerry, I hope that you don’t get penalized for having good control and avoiding complications. The only thing that I can think of is in your appeal, stress how much having the CGMS has helped you be able to maintain the good control. It helps you to be able to exercise as much as you do. That exercise helps to keep you in good shape and prevent problems. Do you have a lot lows without using the CGMS? My A1c was actually 5.3 when I wrote my appeal letter but I was also having a lot of lows so I pointed that out to them.
There is a guy in the Dexcom group on TuDiabetes (his name is Rick) that has helped some people write appeal letters. You might try looking and see if you can get some ideas from him.
Well, I’m grateful that I DON’T have gastroparesis, nor have I ever passed out from a hypo — I usually feel them in the low to mid 50’s. My only excuse is that I’m crazy! What the CGM does for me is alert me to HIGHS, because I don’t feel those, and keeps me on track because I can check easily, and seeing a high makes me feel guilty enough to take my insulin when I’m depressed. So that I don’t land myself in the hospital, nearly dead, like I did in 2010. I don’t know if that would fly with Medicare, but it DID convince my ins. co. to cover it! 🙂
Crazy can get you out of murder but I think Medicare is tougher than a jury! Since you did land in the hospital almost dead, you can probably use that and show how far you have come using the CGMS. So yes, I would use that as a reason. Plus, you don’t know until you try. If you don’t try, you won’t have it unless you can afford to pay for it on your own. The worst they can say is no. You won’t be any worse off than if you didn’t try, but if they say yes, then you get to keep your CGMS. You already had one yes with that reasoning, so there is no reason to think it won’t work again!